We often think of cholesterol levels as a reflection of diet and exercise alone. But there’s another powerful influence many people overlook: stress. Chronic stress doesn’t just affect your mood - it literally rewires how your body handles cholesterol and fats, often leading to elevated LDL cholesterol, even if you eat well and exercise.
Stress Hormones and Cholesterol
When you’re under stress, your body flips into survival mode. Hormones like cortisol and adrenaline are released to keep you alert and fuelled.
- Adrenaline triggers the liver to release glucose, triglycerides, and LDL cholesterol into the blood for instant energy.
- Cortisol helps moderate this release, keeping that fuel available over a longer period.
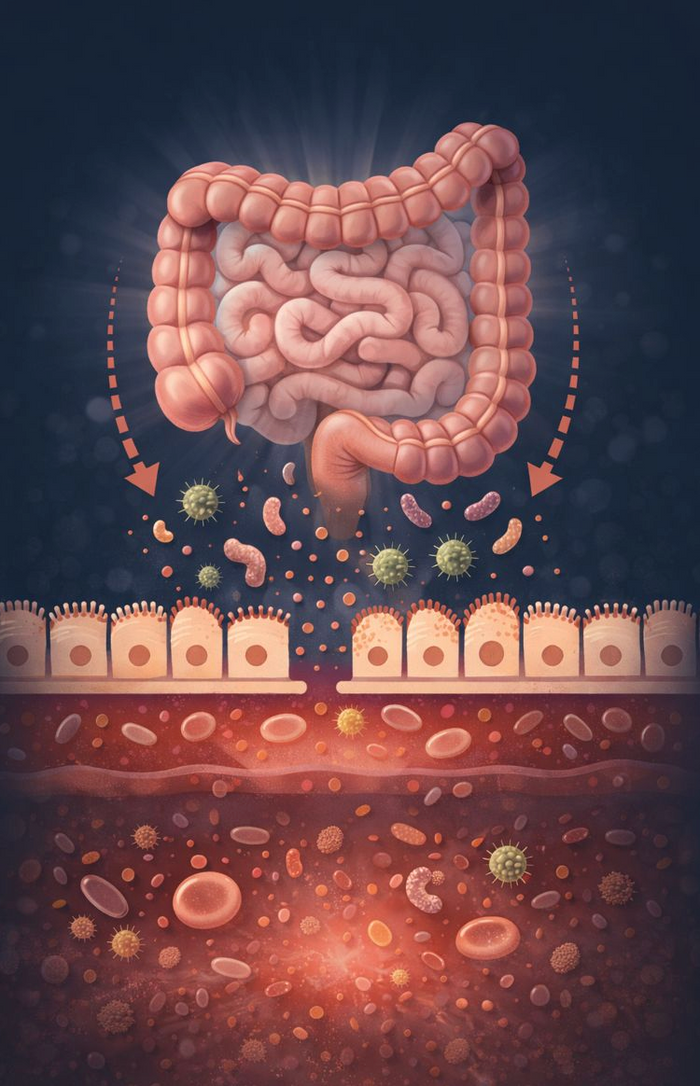
This system once protected us from immediate threats. Today, with stress from emails, deadlines, and arguments, those fats and sugars often linger unused in the bloodstream. Over time, this can lead to higher cholesterol levels and increased cardiovascular risk.
Why Cholesterol Builds Up Under Stress
Stress doesn’t just increase cholesterol production - it also interferes with clearance. Normally, LDL receptors in the liver act like a cleanup crew, removing excess cholesterol from circulation. Under chronic stress, these receptors become less active. Combined with stress-driven inflammation, LDL cholesterol is more likely to oxidise, further raising cardiovascular risk.
The result? Your body produces more cholesterol and clears less of it. This explains why some people have persistently high cholesterol despite a clean diet and regular exercise.
The Adrenal Connection
Cholesterol isn’t just a “bad guy” - it’s the building block for all steroid hormones, including cortisol. Your adrenal glands pull cholesterol directly from LDL and HDL in the blood. If adrenal function is impaired - as it often is with chronic stress or adrenal fatigue - uptake slows. This leaves more cholesterol circulating in the blood.
In practice, that means high LDL cholesterol may not only reflect excess production, but also an inability to use cholesterol effectively.
Nutrient Depletion: Stress Drains the Essentials
Chronic stress also depletes nutrients your body needs to metabolise cholesterol and make hormones:
- Vitamin C - concentrated in the adrenal glands and essential for cortisol production. Chronic stress rapidly drains vitamin C reserves.
- B vitamins (especially B5) - vital for coenzyme A, which drives cholesterol metabolism and hormone synthesis.
- Vitamin A - helps regulate LDL receptors so cholesterol enters cells.
- Magnesium, zinc, selenium, and omega-3s - all support cholesterol metabolism and adrenal health.
When these nutrients are low, cholesterol can’t be processed or used effectively. The result? It builds up in your blood, leaving you with high LDL levels and ongoing fatigue.
Why Testing Matters
If you’re dealing with high cholesterol and chronic stress, the answer isn’t to randomly throw supplements at the problem. The first step is testing. Functional testing can help answer:
- Is adrenal function impaired?
- Are nutrient deficiencies limiting cholesterol use?
- Is cholesterol high due to overproduction, poor clearance, or both?
The Bigger Picture
High LDL cholesterol is rarely just about diet. More often, it’s a sign your body is under pressure - whether from chronic stress, nutrient depletion, or adrenal dysfunction. Supporting your adrenal health doesn’t just help cholesterol; it improves energy, sleep, hormone balance, cardiovascular health, and even mood.
Your bloodwork is telling a story. The real question is: are you listening?
If you’d like further advice on which pathology testing would be most appropriate for you, please ask the team at support@astonrx.com