If you’ve been checking your Met-Flex graph and noticed you’re mostly (or always) in Glucose Mode, you’re not alone - and it’s not a failure.
In fact, for many people, especially women in midlife, this is simply the starting point.
Let’s unpack what it really means, why it happens, and how to move forward without extreme measures.
First: Glucose Mode is not “bad”
Glucose Mode simply means:
Your body is relying more on sugar than fat for fuel right now.
That can be completely normal and appropriate in many situations, including:
- after eating carbohydrates
- during stressful periods
- with poor sleep
- during hormonal transitions (peri- or post-menopause)
- when insulin resistance is present
It does not mean:
- you’re metabolically broken
- you can’t burn fat
- your efforts aren’t working
It means your body is currently choosing the most available fuel.
Why many people stay stuck in Glucose Mode
There are a few common reasons Glucose Mode dominates:
1. Carbohydrates are frequent and late in the day
Carbs aren’t “bad” - but when they’re:
- eaten often,
- combined with higher fat,
- or concentrated in the evening,
they can keep glucose elevated and ketones suppressed.
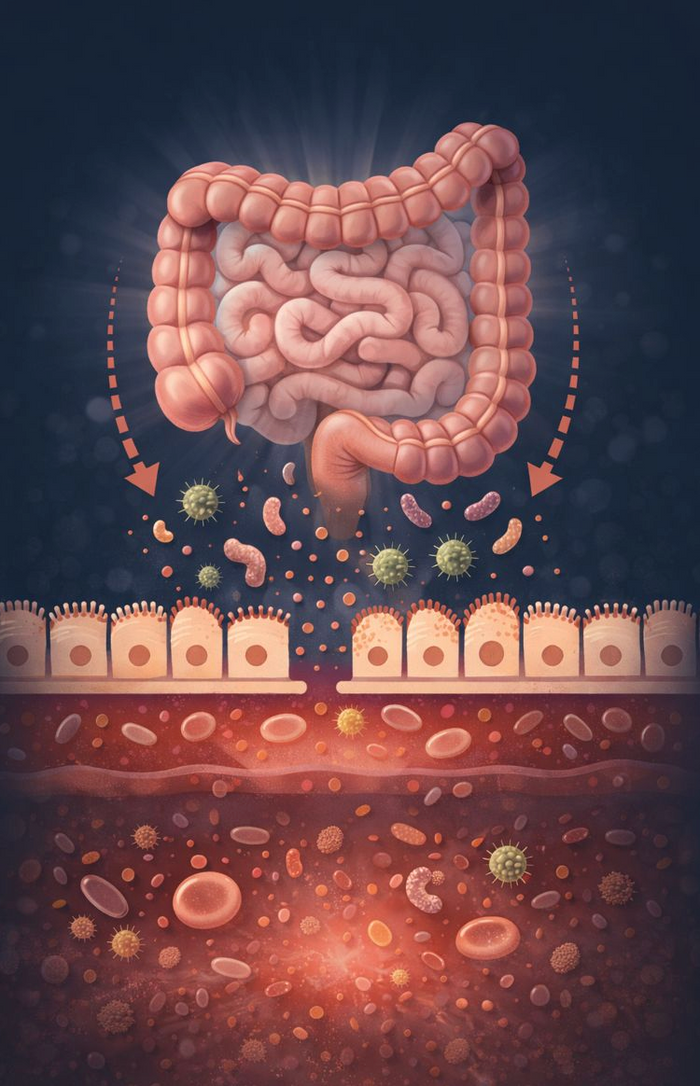
2. Insulin resistance (very common, often hidden)
If insulin stays high, the body:
- struggles to access stored fat,
- suppresses ketone production,
- and defaults to glucose use.
This is especially common in:
- elevated stress/poor sleep
- people with long dieting histories
- those with central weight gain
Stress and poor sleep
Cortisol raises glucose and blocks fat access - even if your food is “perfect”.
Many people see:
- higher GKI readings after poor sleep
- stubborn Glucose Mode during stressful weeks
This is physiology, not willpower.
4. Protein overload (yes, it matters)
Protein is essential - but very high protein, especially spread across all meals, can:
- raise glucose via gluconeogenesis
- keep ketones lower than expected
More is not always better.
What actually helps you move out of Glucose Mode
You don’t need to jump straight to extreme fasting or keto.
Small, strategic shifts create the biggest wins.
Build short “fat-access windows”
You don’t need Fat Mode all day.
Try:
- a 12–14 hour overnight eating break
- or one day per week where you skip a meal
- or an earlier dinner several nights a week
These windows teach your body how to access fat again.
Walk after meals
A simple 10–15 minute walk after meals:
- lowers post-meal glucose
- improves insulin sensitivity
- makes it easier to see movement into Flex Mode
This is one of the most underrated tools.
Support sleep and stress first
If sleep is poor or stress is high:
- glucose will stay elevated
- ketones will stay suppressed
Improving sleep quality can shift your Met-Flex score without changing food at all.
Aim for Flex Mode, not Fat Mode (at first)
This is crucial.
Flex Mode is success.
It means:
- glucose is controlled
- ketones are present
- your body is learning to switch fuels
Most people should aim to:
spend more time in Flex Mode before chasing Fat Mode
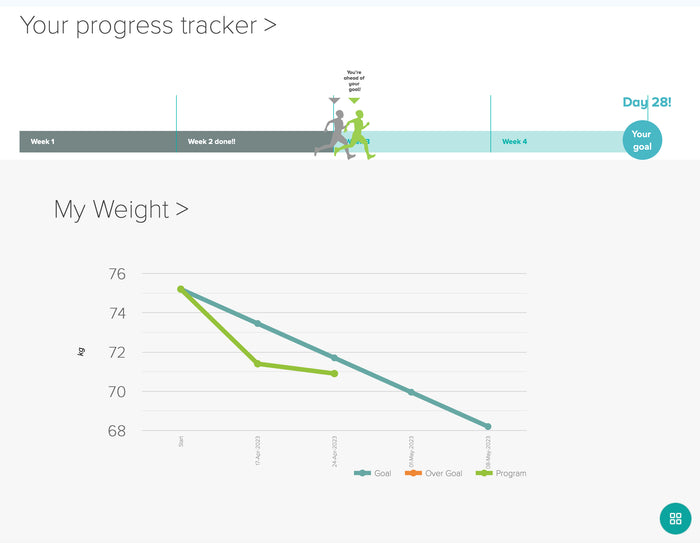
What progress usually looks like
Healthy progress often follows this pattern:
- Less time in high Glucose Mode
- More frequent Flex Mode readings
- Occasional Fat Mode “appearances”
- Easier switching between zones
This can take weeks to months, especially if insulin resistance or hormonal changes are involved.
That’s normal — and sustainable.
The key mindset shift
The Met-Flex graph is not a grade.
It’s a map.
Glucose Mode shows where you are today.
Flex Mode shows momentum.
Fat Mode shows capacity — not a permanent destination.
Bottom line
If you’re always in Glucose Mode:
- you’re not failing
- you’re learning
- and you’re exactly where change begins
Focus on patterns, not perfection, and let your Met-Flex graph guide smarter, calmer adjustments over time.