A groundbreaking new study says yes — especially if you’re a woman.
Published recently in JAMA Psychiatry, the research reveals a significant link between soft drink consumption and increased risk and severity of major depressive disorder (MDD) in women. Even more intriguingly, the findings suggest this connection may be driven, at least in part, by changes in the gut microbiome — specifically, an overgrowth of a little-known bacterium called Eggerthella.
THE STUDY: SOFT DRINKS & MENTAL HEALTH
Led by Dr. Sharmili Edwin Thanarajah of the University Hospital Frankfurt, the study included 932 participants, of whom 405 had clinically diagnosed MDD. Researchers examined soft drink intake and analyzed gut bacteria in stool samples to explore whether diet might influence mental health via the gut-brain axis.
The results?
- Women who consumed more soft drinks had a 16.7% higher risk of developing MDD, and experienced more severe symptoms.
- This association was significantly mediated by increased levels of Eggerthella — a gut bacterium linked to inflammation and mood disorders.
- The gut changes explained 3.8% of the increased MDD risk and 5% of symptom severity.
While the overall effects might sound small, the widespread consumption of soft drinks makes this a meaningful public health issue.
WHY IT MATTERS FOR WOMEN
Interestingly, the effects were not observed in men.
Dr. Thanarajah suggests hormonal differences or the so-called "microgenderome" — the interaction between gut microbes and sex hormones — may help explain why women are more vulnerable to these effects.
Other studies have consistently shown:
- Women are more susceptible to depression than men.
- Women are more affected by dietary triggers like soft drinks and ultra-processed foods.
- Gut bacteria such as Eggerthella may impact the brain differently depending on sex.
HOW SOFT DRINKS DISRUPT THE GUT
So, what makes soft drinks so uniquely problematic?
“Unlike solid food, soft drinks deliver a rapid hit of sugar or sweeteners to the colon, promoting the growth of pro-inflammatory bacteria and spiking blood sugar,” said Dr. Thanarajah.
This imbalance may increase inflammation, disrupt neurotransmitters, and ultimately impact mood.
Key factors:
- Sugars like glucose and fructose can overwhelm the small intestine’s ability to absorb them.
- Artificial sweeteners, such as aspartame and saccharin, may also disrupt gut microbes.
- These gut changes may influence the brain’s reward system, reinforcing cravings and mood symptoms.
A PUBLIC HEALTH WARNING
Dr. Thanarajah believes it’s time to bring dietary habits into the spotlight when assessing mental health.
“Physicians should consider asking patients about soft drink consumption as part of routine dietary assessment, especially in those with or at risk of depression.”
WHAT ABOUT DIET SOFT DRINKS?
The study didn’t differentiate between sugar-sweetened and artificially sweetened soft drinks — but both were linked to gut changes. More research is needed to clarify if certain ingredients (like high-fructose corn syrup vs. aspartame) are worse than others.
What’s clear is that both types may disturb gut balance in ways that negatively affect mental health — especially for women.
FOOD FOR THOUGHT (AND MOOD)
This research adds to a growing body of evidence supporting the gut-brain connection and reinforces what AstonRX practitioners see regularly:
What you eat affects how you feel.
Soft drinks, often dismissed as harmless indulgences, may be quietly eroding mental and metabolic health — not just through sugar and calories, but by feeding the wrong bacteria in the gut.
WHAT YOU CAN DO
If you're concerned about mood, energy, or gut health, consider the following:
- Replace soft drinks with sparkling water or herbal teas.
- Prioritise whole foods that nourish a healthy microbiome.
- Track your symptoms when you cut out sweetened beverages — you might be surprised how quickly your mood lifts.
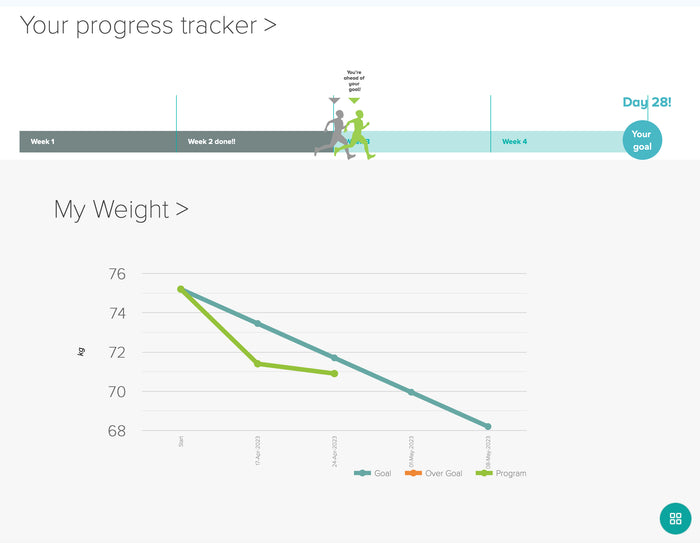
At AstonRX, we help our members restore metabolic and mental health by rebalancing the gut and removing inflammatory foods and drinks — soft drinks included.
The science is catching up to what we’ve known anecdotally for years: When you support the gut, the brain follows.
Sources:
- JAMA Psychiatry (Sept 2025)
- Medscape Medical News
- Interview with Dr. Sharmili Edwin Thanarajah
- Commentary by Dr. Uma Naidoo, Harvard Medical School