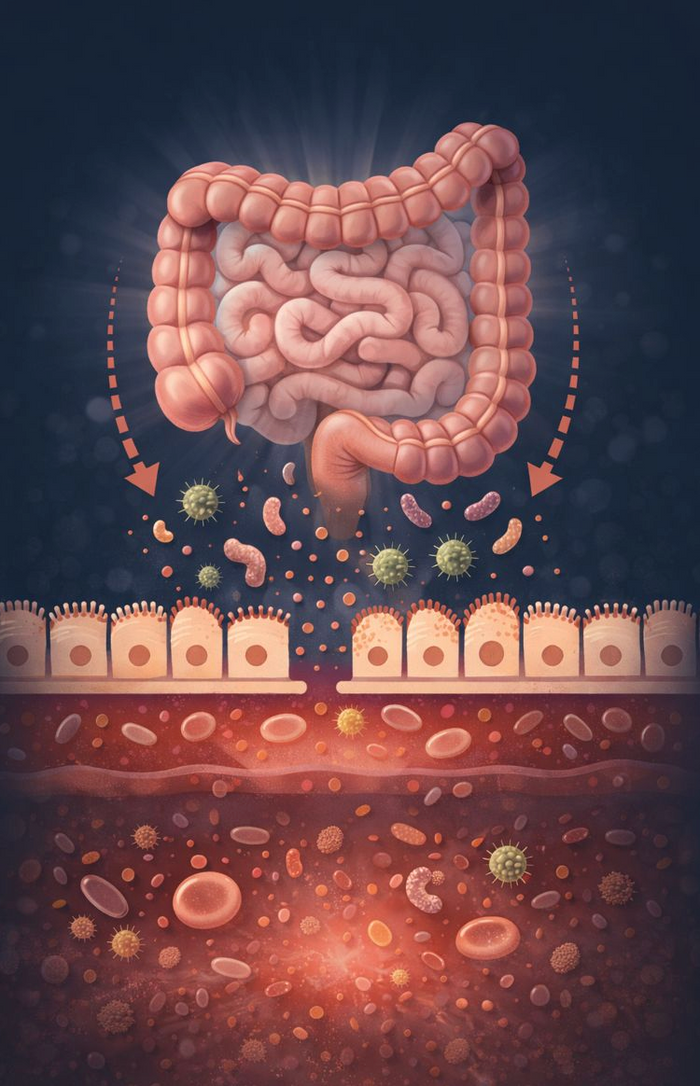
Insulin resistance (IR) is emerging as one of the strongest risk factors for cardiovascular disease (CVD), yet its connection to commonly prescribed medications is often overlooked. Many blood pressure (BP) medications, while effective at reducing BP, can exacerbate IR, potentially undermining their benefits.
Blood Pressure Medications and Insulin Resistance
-
Beta Blockers:
Beta blockers suppress the sympathetic nervous system, dampening the "fight or flight" response triggered by adrenaline. Unfortunately, this increases IR. Side effects such as sleep disturbances, fatigue, cold extremities, and depression are common, and the resulting metabolic dysfunction can compound cardiovascular risks. -
ACE Inhibitors:
ACE inhibitors prevent the enzyme that causes vasoconstriction, reducing blood pressure by promoting water excretion via the kidneys. While effective, they increase the risk of dehydration, potassium retention, and sodium loss, potentially disrupting electrolyte balance. Such imbalances can lead to increased insulin levels and further IR. -
Calcium Channel Blockers:
By blocking calcium from entering cells, these medications relax blood vessels. However, side effects like headaches, dizziness, and oedema are common. They may also impair mitochondrial function, essential for energy production and metabolic health. -
Diuretics:
Diuretics force the kidneys to expel salt and water, but this can disrupt electrolytes, leading to neurological issues, muscle cramps, and increased IR. They are also linked to Type 2 diabetes (T2DM). Additionally, restricting salt can paradoxically trigger the body to increase insulin levels to stabilise sodium, worsening IR.
Cholesterol: Misunderstood in Heart Health
Cholesterol, particularly LDL (low-density lipoprotein), is often labelled a villain in heart disease. However, the reality is nuanced. LDL itself isn't harmful until oxidised, a process influenced by the composition of fats within LDL molecules. Saturated fats are stable and resist oxidation, while polyunsaturated fats (PUFAs) oxidise rapidly, driving inflammation.
Interestingly, LDL acts like a "fire truck," responding to injuries and infections. Low LDL levels have been associated with a higher risk of severe infections. Emerging treatments like PCSK9 inhibitors and statins lower LDL levels but come with trade-offs: increased IR, mitochondrial dysfunction, muscle pain, and reduced GLP-1, which affects glucose regulation.
A Balanced Approach to Longevity
Studies, including a 35-year Swedish study, suggest that higher LDL levels and low blood glucose levels are associated with exceptional longevity and reduced CVD risk. Addressing insulin resistance through lifestyle changes, rather than over-reliance on medications, may offer a more effective path to long-term heart health.
Find out more about the pathology testing here