Why we deserve better conversations, better testing, and better choices
Bone health is something many women do not think about until a scan, a fracture, or a prescription forces the issue. That was certainly my experience.
I have a strong maternal history of osteoporosis. I knew it mattered, but like many women, it sat quietly in the background while life, work, and health priorities took centre stage.
In 2020, I suffered a back injury that was genuinely debilitating. It significantly reduced my ability to strength train for a period of time. Coincidentally, this injury occurred during my early 50s, a stage of life when hormonal changes accelerate, particularly the decline in oestrogen that normally protects our bones.
Those two factors combined reduced mechanical loading on my skeleton at the very time my hormonal protection was falling.
My first DEXA scan and a familiar story
In 2022, at 55 years old, I had my first DEXA scan to measure bone mineral density. I was surprised when the result came back as osteopenia, the stage before osteoporosis.
When my GP received the report, the response was immediate and very brief. I was prescribed a pharmaceutical medication for bone density, with no discussion about nutrition, supplementation, strength training, hormones, lifestyle, or even my vitamin D levels. I later spoke with another doctor colleague who supported my decision to manage my bone health, at least for the foreseeable future, using my knowledge of nutrition, training, and lifestyle. He said, Donna, I know you will train hard and consistently, so if anyone can manage their bone health without medication, it is you. That is exactly what I have done, and what I have continued to do ever since.
I speak with women every single day who tell me the same story. Some have already had fractures. Some are taking medications with significant side effects. Most have never had their vitamin D measured. Many have never been told how critical progressive strength training is for bone health.
That is why I am sharing my story. Women deserve to understand their options and to have informed, confident conversations with their doctors and allied health professionals.
Osteoporosis medications and what women are rarely told
In Australia, the most commonly prescribed osteoporosis medications fall into two main categories.
Bisphosphonates
Examples include alendronate, risedronate, and zoledronic acid.
These drugs work by slowing bone breakdown.
Common concerns and side effects can include:
- Gastrointestinal irritation
- Muscle and joint pain
- Suppression of normal bone remodelling with long term use
- Rare but serious risks such as osteonecrosis of the jaw and atypical femur fractures, particularly relevant for women needing major dental work
Denosumab (Prolia)
This is an injectable medication given every six months.
It also reduces bone breakdown but through a different pathway.
Important considerations include:
- Rapid bone loss if the drug is stopped without follow up treatment
- Ongoing dependency on the medication
- Similar jaw and dental concerns
These medications can improve bone density on scans, but fracture risk reduction varies, and they do not address the underlying drivers of bone loss.
How does this compare to hormone replacement therapy
For women in early menopause or post menopause, hormone replacement therapy deserves serious consideration.
Even at low doses, oestrogen has been shown to:
- Reduce bone loss
- Lower fracture risk
- Support muscle mass
- Improve insulin sensitivity
- Offer cardiovascular protection when started at the right time
For many women, HRT has fewer side effects than osteoporosis drugs and offers multiple systemic benefits beyond bone alone. Yet it is often not discussed as an option.
Discovering the importance of TBS and quality imaging
Recently, I had the pleasure of meeting a highly skilled Clinical Densitometrist at Arekai Imaging. This conversation changed how I view bone testing entirely.
Who knew that not all DEXA scans are equal? Differences in equipment, software, and technician expertise matter. Importantly, not all clinics offer Trabecular Bone Score, or TBS.
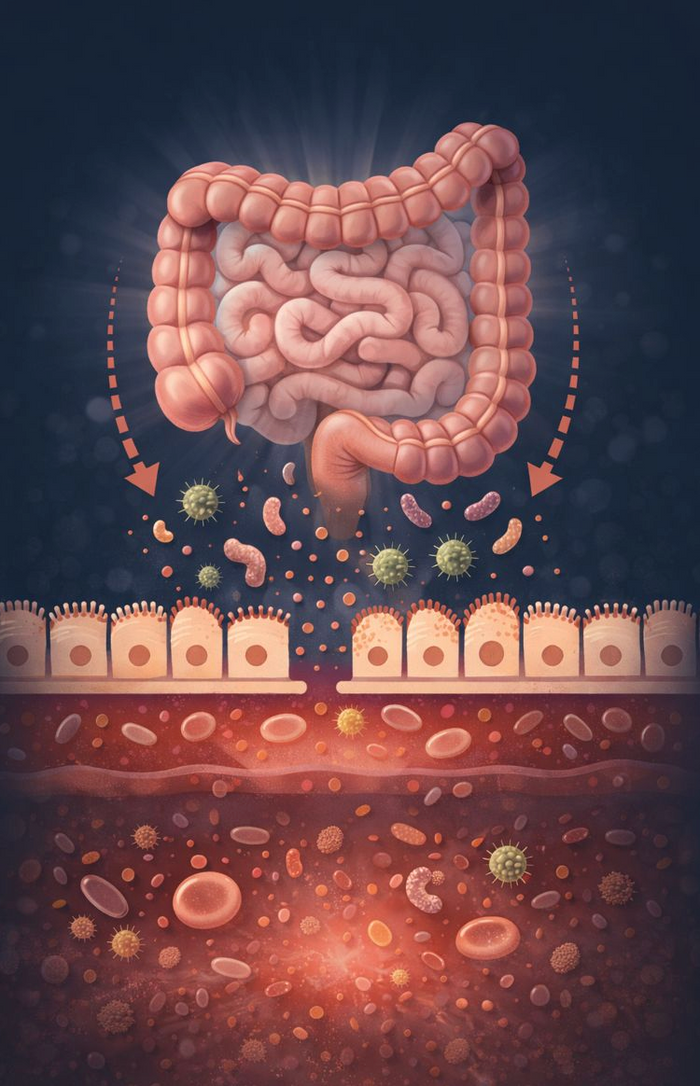
TBS assesses bone microarchitecture. In simple terms, it looks at the internal structure of bone, not just how dense it is. Density tells part of the story. Structure tells us how strong and resilient the bone actually is.
Here is why this matters.
Low BMD plus degraded or partially degraded TBS
This is the classic osteoporosis pattern where both density and structure are compromised.
- Common in postmenopausal women, older men, or those with long term bone loss
- Fracture risk is high and TBS reinforces that risk
Low BMD plus normal TBS (this is me!)
This suggests low peak bone mass but preserved internal structure.
- Often seen in smaller or lean individuals, including some athletes
- Fracture risk may be lower than the T score alone suggests
Normal BMD plus degraded or partially degraded TBS
This is less common but extremely important.
- Seen in people with type 2 diabetes, inflammatory conditions, or long-term steroid use
- Density looks reassuring, but bone quality is compromised
- TBS uncovers hidden fragility
Osteopenic BMD plus partially degraded TBS
- Common in early menopause or age-related bone loss
- TBS can influence whether early intervention or closer monitoring is needed
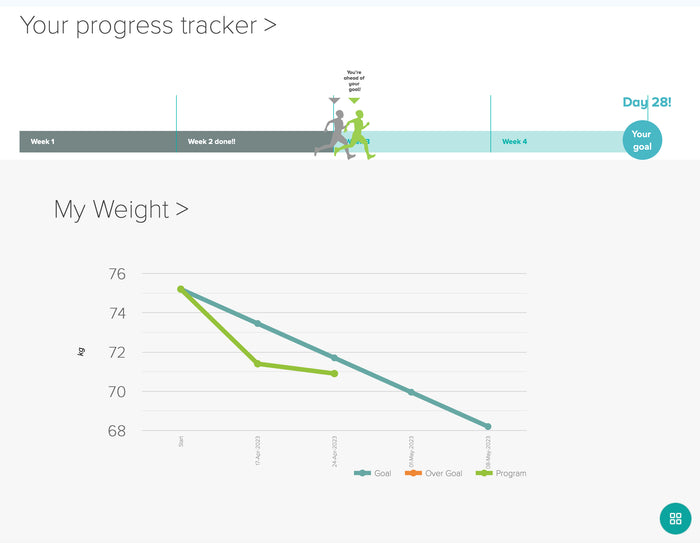
My most recent results and what they actually mean
I had not had my bone density measured since 2023, so this year I booked a repeat DEXA with TBS at Arekai.
The results were reassuring. My bone mineral density remains in the osteopenic range, but it has improved slightly since 2023. More importantly, my TBS was in the normal range.
That means my bone architecture is intact. My fracture risk is lower than my density alone would suggest. This changes the conversation entirely.
This is exactly why women need better testing and better interpretation, not reflex prescriptions.
Strength training is non-negotiable for bone and muscle
Progressive load strength training is one of the most powerful tools we have to protect bone and prevent sarcopenia.
Bone responds to load. Muscle pulls on bone. Without sufficient mechanical stress, bone deteriorates.
This is now even more important as we see increasing use of GLP-1 medications. While these drugs can support weight loss, they also increase the risk of muscle and bone loss if strength training and protein intake are not prioritised.
Walking, yoga and/or Pilates alone is not enough. Steps are valuable for health, but they do not replace progressive load resistance training for bone integrity. We need to lift heavy stuff!
Supplementation and blood testing matter
Vitamin D is foundational for calcium absorption and bone health. Yet most women have never had their levels tested.
Optimal year-round blood levels sit around 100 to 150 nmol/L, not just barely in range.
Supporting nutrients include:
- Vitamin K2 to help direct calcium into bone
- Magnesium for vitamin D metabolism and bone structure
- Adequate dietary calcium rather than excessive supplementation unless indicated
Supplementation without blood testing is guesswork. Testing allows precision.
Medications that affect bone deserve closer monitoring
Certain medications directly impact bone density. Thyroxine is a common example. Long term or excessive dosing can accelerate bone loss.
This makes regular bone density testing, blood work, and consistent strength training even more important for women on these medications.
A practical takeaway for every woman
When your GP refers you for a DEXA scan, ask the clinic one simple question:
Do you include Trabecular Bone Score with your measurements?
If they do not, find a clinic that does.
Density alone does not tell the full story. Bone quality matters.
A final word
Osteopenia and osteoporosis are not just conditions to be medicated. They are signals to look deeper.
Women deserve informed choices, individualised care, and conversations that go beyond prescriptions. My hope in sharing this story is that more women feel empowered to ask better questions, understand their results, and take charge of their bone health with confidence.
Your bones are living tissue. How you nourish them, load them, and support them matters.
And you are allowed to expect more from the system that cares for you.
If you'd like some recommendations for health and medical professionals, we suggest that you start with booking with our General Practitioner, Dr Charlton.
Bookings available (telehealth or in person) HERE.