A Gut Feeling
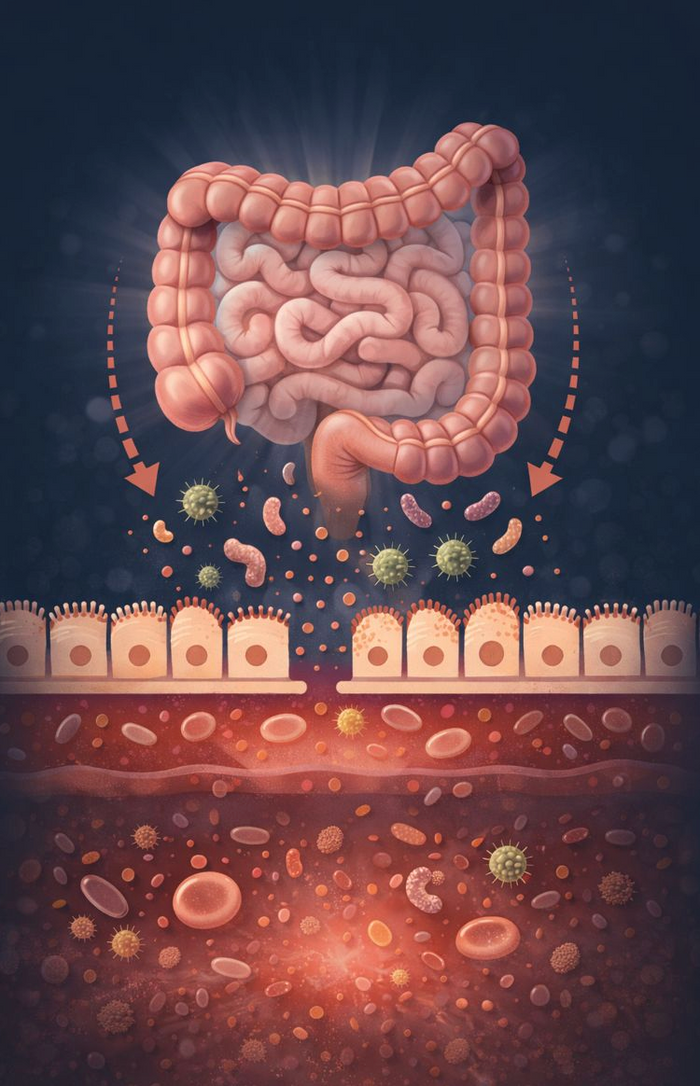
You have over 100 trillion microbes living inside your body, collectively known as your microbiota. Amazingly, your body contains more bacteria than it does human cells, which play a significant role in your overall physical and mental wellbeing. When you consider that 80 percent of your immune system is based in your gut, it reinforces the importance of caring for and protecting your gut health. Intestinal dysbiosis is a condition in which the bacteria in your gut are out of balance, and pathogenic (bad) bacteria begin to dominate, potentially jeopardising your physical and/or mental wellbeing. The composition and balance of our gut microbiota differs among individuals, but to remain healthy, certain bacteria should dominate and act to suppress the overgrowth of harmful bacteria. The symptoms stemming from dysbiosis are many, including abdominal bloating and cramping, constipation, diarrhea, indigestion, reflux, heartburn, food intolerances and sensitivities, excessive weight gain, fatigue, brain fog, lowered mood, joint pain, inflammation and numerous common skin conditions. Many of these symptoms are often misunderstood and therefore not recognised as dysbiosis. They’re commonly treated with pharmaceuticals, some of which can actually worsen gut flora.
What are some of the causes of intestinal dysbiosis?
- Antibiotics
- Poor dietary habits (high sugar/refined foods, low fibre, etc.)
- Chronic stressGastrointestinal infections (food poisoning, traveler’s diarrhea, gastroenteritis)
- Pharmaceuticals, such as NSAIDs, proton pump inhibitors
- Altered gastric secretions (gastric acid, pancreatic enzymes, bile)
- Excessive alcohol consumption
Food intolerances and sensitivities
Nowadays, you can’t swing a cat without hitting someone with a food intolerance! Something that was almost unheard of 30 years ago. Whether medically diagnosed, or self-diagnosed with the assistance of good old Dr. Google, there is no doubt that these sensitivities are far more prevalent than ever before.
The most common ‘cure’ is to establish a list of the culprits (commonly lactose, fructose, gluten, etc.) and avoid them like the plague.
I prefer to find the reason for this reaction rather than simply putting a band aid on it. You may find that your gut bacteria area contributing factor.
For example, certain strains of bacteria are responsible for the production of lactase –the enzyme required to digest lactose (found in milk). If you are deficient in these bacteria, it makes sense that you’d have trouble digesting milk products. So, do you simply avoid dairy (and the bone-building calcium it provides), or do you rebuild your gut flora to remedy the problem? We now know so much more about a myriad of different strains of gut bacteria, specific to various health issues, from urinary-tract infections to mood disorders. It is said that our gut is our second brain and I believe this will become increasingly relevant in the diagnosis and treatment of disease as research continues to evolve.
Gut-brain connection
Most of us have experienced feeling unsettled in our gut during times of stress. Nausea, diarrhoea and indigestion are all commonly related to stress and anxiety. The concept of the gut influencing the brain, and vice-versa, is not new. However, previous attention has been focused on gut-specific behaviours, such as hunger and satiety. More recently, studies have linked the gut-brain axis to moods and behaviour independent of eating, with suggestions that the microbiota is the key regulator of the gut-brain connection, with influence on anxiety, low mood and stress. One very important role of your gut flora is to communicate with the central nervous system. The ability of these two systems to communicate effectively is emerging as a critical factor in health and disease.
So how can I improve my gut microbiota?
1. Starve the ‘bad’ bacteria by eliminating sugar and refined foods from your diet
2. Increase your consumption of fibre-rich plant foods
3. Consider taking a daily probiotic supplement (broad spectrum, live bacteria)
4. Consider a prebiotic fibre supplement (ferments in your gut to ‘feed’ the ‘good’ bacteria) If symptoms persist, it’s always advisable to seek guidance from a qualified health professional.
There are now several methods available to medically diagnose your current microbiota and accurately identify and treat intestinal dysbiosis.