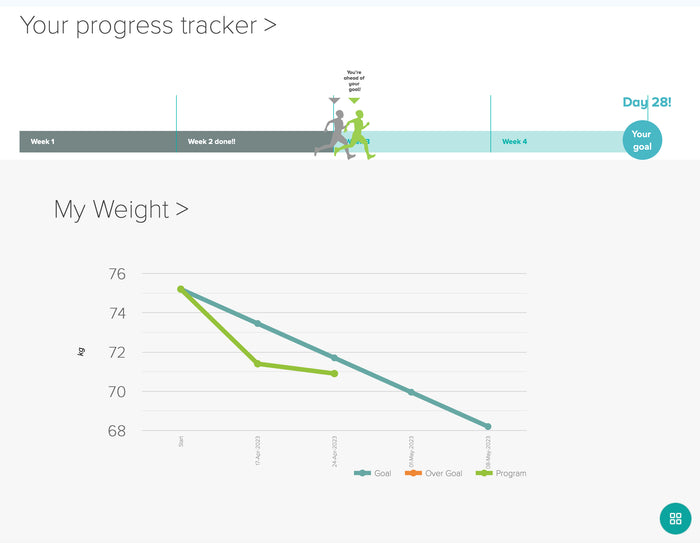
How Does Insulin Resistance Cause PCOS?
The cells in our ovaries produce some of our essential hormones, including oestrogen and progesterone. These cells also secrete a small amount of testosterone. Testosterone is actually essential for many bodily functions, including libido and bone formation.
if you have really high insulin levels all the time then it causes your ovaries to overproduce testosterone. Our bodies usually have a system in place which prevents hormone levels from getting too high. Unfortunately this isn’t the case with testosterone and our bodies also don’t anticipate insulin making testosterone levels higher. As a result, there’s nothing to prevent testosterone levels spiraling out of control.
It doesn’t just end there though. When it comes to hormones, 80% should be bound to cells and 20% should be free in the body. The ‘free’ hormones are generally the ones which cause problems. Excess levels of ‘free’ testosterone can:
– Get into hair follicles and make hair fall out.
– Settle in hair follicles in our face and make it produce thick dark hair.
– Get into skin glands and cause acne.
In most people, Sex Hormone Binding Globulin (SHBG) acts as a testosterone ‘sponge’, binding to excess testosterone and preventing it from causing these problems. However, insulin resistance reduces the amount of SHBG, thereby increasing testosterone levels. You can think about insulin resistance as a delinquent child. He has put the plug in the bath, turned the testosterone taps on, stolen your sponges, and run away calling ‘catch me if you can!’
How Do Insulin Resistance and PCOS Affect Pregnancy?
The one thing you need to get pregnant is an egg that’s reached maturity and been released (ovulation). If your ovaries haven’t released any eggs then there is nothing to meet the sperm, stopping you from getting pregnant. Ovulation is controlled by a delicate balance of hormones.
After your period your body starts to prepare some baby eggs (follicles) to mature and be released. Contrary to popular belief, it’s actually many eggs (not one) so that the body has some backups. You can think of these eggs like Russian dolls. It’s not that they fit inside each other, but there are many of different sizes that are being prepared at different stages for ovulation. This part of the ovulation process is controlled by Follicle Stimulating Hormone (FSH). FSH stimulates the follicles to mature.
Once the biggest follicle is ready, it signals this to the body and Luteinizing Hormone (LH) is released. When Luteinizing Hormone reaches peak level, it will release the egg into the uterine tube. The egg is then ready for a conjugal visit from some awaiting sperm.
Anything that disrupts the processes of the egg’s maturity or release will stop ovulation. Scientists still don’t know exactly how insulin resistance and PCOS affects these processes. However, insulin has been shown to affect the following three things:
Insulin Affects the Delicate Hormone Balance
LH is like the switch for ovulation: you can only ovulate when your LH rises steeply. However, researchers think that the ratio of LH to FSH is the thing that’s really important for ovulation. Studies on PCOS have shown that insulin increases LH, damaging the LH:FSH ratio. Clomid is a drug which is given to many women with PCOS who are struggling to ovulate. Clomid increases FSH levels and re-balances the ratio.
Insulin Suppresses FSH
As I mentioned above, FSH’s role is to develop one of those ‘Russian Doll’ follicles into an egg. However, insulin resistance suppresses FSH. This means that all eggs are the same size and there isn’t a ‘superior’ one to be released into the uterine tube. These undeveloped follicles are what appear as ‘cysts’ on our ovaries.
Insulin Stops Follicles Developing Properly
High levels of insulin in the blood increase testosterone levels. Studies have shown that if follicles are exposed to too much testosterone when they are forming then they won’t develop properly. This is another way that too much insulin can impact pregnancy.
Why Do Some Women Have Insulin Resistance, But Not Develop PCOS?
Scientists still don’t know the answer to this question but think that this is where genetics play a part. Studies have shown that there is a genetic component to PCOS and have identified which genes are most likely involved. These genes may make our ovaries and adrenal glands more sensitive to insulin and make them produce more androgens.
Having these genes doesn’t mean that you’re doomed. Studies have also shown that genes can be turned on and off by environmental factors. This is called epigenetics. We therefore need to remove these environmental factors to turn the PCOS genes off.
What Causes Insulin Resistance?
This is by no means an exhaustive list but here are some of the main causes of insulin resistance:
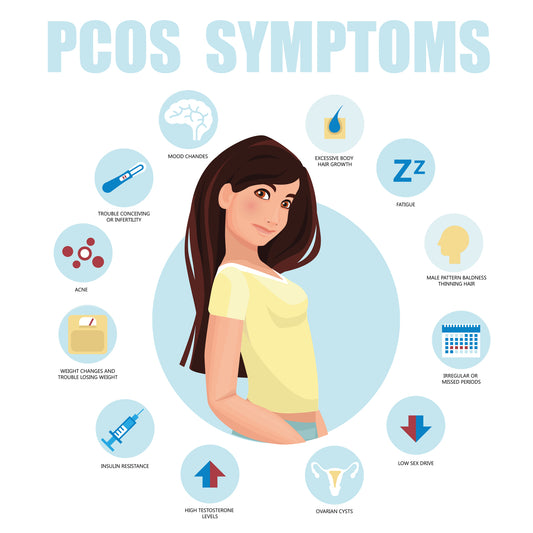
Inflammation (and Sugar)
You know how you’ve read (or may have been told by your doctor) that insulin resistance is caused by being lazy and eating too many sweets? Although these definitely contribute, eating too many refined carbohydrates isn’t the only cause.
Sugar is mostly to blame, but inflammation also plays a big part. Studies have now shown that inflammation can cause insulin resistance and may need to be present for insulin resistance to occur in the first place. Inflammation is a normal feature of our immune system and is critical for our survival. Problems arise when our immune system is chronically activated. This chronic inflammation damages our cells.
Women with PCOS have significantly higher levels of inflammatory blood markers than ‘normal’ women. It is also thought that PCOS is an inflammatory condition, like obesity, diabetes, heart disease, and cancer.
If you have insulin resistance and PCOS, then you almost certainly have inflammation. This is very important when considering PCOS treatment and is the reason why simply removing carbs isn’t effective for many women. Inflammation also needs to be treated.
For the purposes of this article, I’ll use the term ‘insulin resistance’, but you should read it as 'inflammatory insulin resistance.'
The Birth Control Pill
Yes, the hormones that you’re given as a treatment for PCOS could actually be causing it. The pill that you’re given to ‘regulate your period’ can cause insulin resistance. A recent study of 42 women found that the pill caused inflammation and the beginnings of insulin resistance. This was after just 9 weeks of taking it.
As a side note, I wrote ‘regulate your period’ in inverted commas because the pill can never regulate your period. The pill causes a ‘pill bleed’, not a real period. A period is a withdrawal bleed from the hormones estradiol and progesterone (made by your ovaries). A pill bleed is a withdrawal bleed from pharmaceutical steroids, such as ethinylestradiol and levonorgestrel. The pill masks the problem and you still won’t have a regular period once you come off it.
Not Enough Sleep
Studies have shown that a lack of sleep can directly reduce insulin sensitivity. One study took two groups of men and put them in a hospital setting so they could control everything, from what they ate to how much they exercised. The amount of sleep that they had was the only thing that was manipulated.
When their sleep was reduced down to 5 hours a night, the men’s insulin sensitivity was
reduced by 24%. This proves that you could be doing everything ‘right’ in regard to diet and exercise, but if you’re not sleeping enough then you are still going to be developing insulin sensitivity.
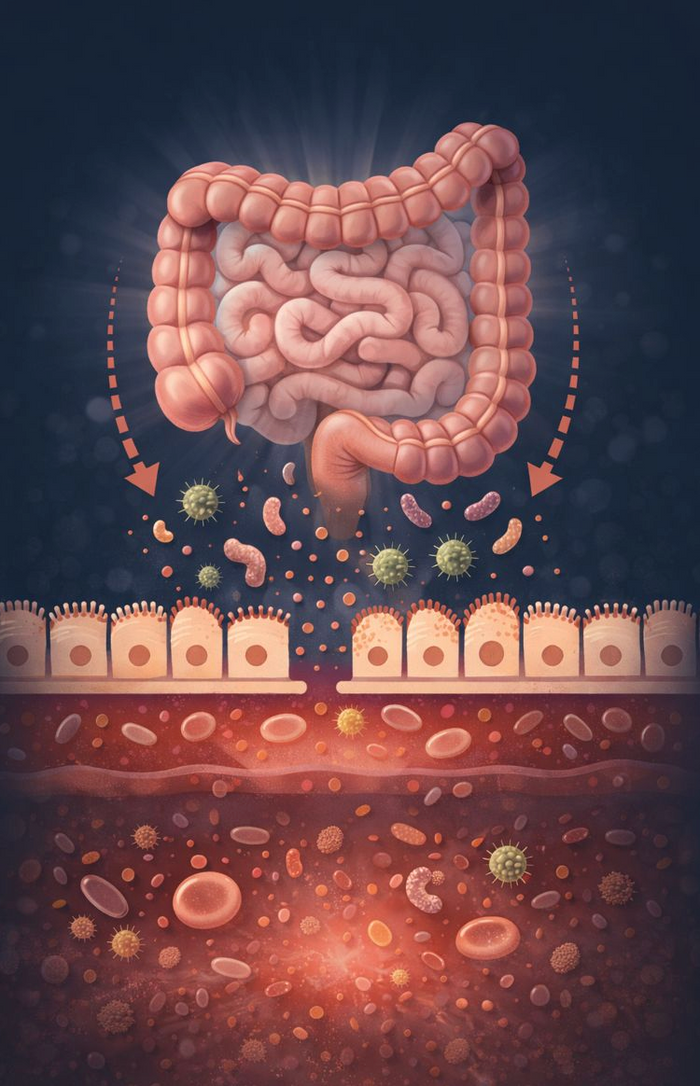
Imbalanced Gut Bacteria (Microbiome)
The microbiome is the name given to the bacteria, viruses, fungi, and protozoa that live throughout your body, specifically in your gut. It’s responsible for many different functions in the body, including 75% of our immune system. It is also directly responsible for how many calories and carbs we extract from our food.
This bacteria is completely normal, but problems arise when there is too much bad bacteria or not enough good bacteria. Too much bad bacteria causes too much insulin to be produced, leading to insulin resistance. Women with PCOS also have fewer good bacteria and more bad bacteria than normal.